Scaling standardized protocols saved one hospital $12M in 1 year
Value-based care delivery is dependent on perioperative value.
Approximately 45 to 60 percent of a hospital’s revenue and expenses are related to perioperative services, and bundled payment models demand standardization and reliability to be successful. Yet at many hospitals, high variability in outcomes and costs produces a misalignment of goals among physicians, staff and administrators.
Besides delayed cases, slow operating room throughput, dissatisfied surgeons and significant deviations between same procedures performed by different surgeons inhibit organizations from offering competitive pricing or assuming the financial risk of managing community health.
At Wilmington, N.C.-based New Hanover Regional Medical Center, North American Partners in Anesthesia's team led by Rob Shakar, MD, chief of anesthesia, worked collaboratively with clinical colleagues to improve standardization in the total joint program by piloting a perioperative surgical home program in orthopedics.
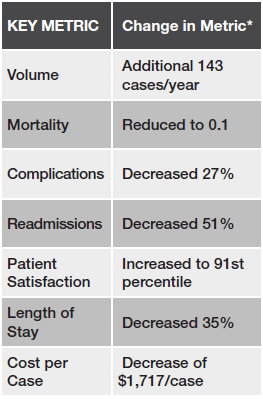
The program generated outstanding clinical and operational outcomes and saved the hospital $4.2 million in the first year, prompting the hospital to scale perioperative surgical home across 16 service lines that produced an annual return on investment of up to $12 million.
Download this case study to learn:
Approximately 45 to 60 percent of a hospital’s revenue and expenses are related to perioperative services, and bundled payment models demand standardization and reliability to be successful. Yet at many hospitals, high variability in outcomes and costs produces a misalignment of goals among physicians, staff and administrators.
Besides delayed cases, slow operating room throughput, dissatisfied surgeons and significant deviations between same procedures performed by different surgeons inhibit organizations from offering competitive pricing or assuming the financial risk of managing community health.
At Wilmington, N.C.-based New Hanover Regional Medical Center, North American Partners in Anesthesia's team led by Rob Shakar, MD, chief of anesthesia, worked collaboratively with clinical colleagues to improve standardization in the total joint program by piloting a perioperative surgical home program in orthopedics.
The program generated outstanding clinical and operational outcomes and saved the hospital $4.2 million in the first year, prompting the hospital to scale perioperative surgical home across 16 service lines that produced an annual return on investment of up to $12 million.
Download this case study to learn:
- The benefits of monetizing the perioperative surgical home program
- How perioperative surgical home program can increase operating room utilization, first case on-time starts and patient and surgeon satisfaction
- How a perioperative surgical home program has decisive impacts on patients, surgeons, efficiency and profitability
Please fill out the form to download the whitepaper.