Revolutionizing Utilization Review for
Greater Sustainability
Wednesday, July 17th, 2019 | 12:00pm - 1:00pm CT
The utilization review area of the revenue cycle has been experiencing changing dynamics and contributing factors which require new thinking in order to optimize it. These factors include a sharp increase in medical necessity denials, a decrease in the success rate of commercial denial overturns, and the ongoing need for revenue integrity to combat providers’ margin pressures.
Infusing artificial intelligence (AI) and rethinking utilization review processes is emerging as an answer to enhancing this critical part of the revenue cycle to help with overall provider sustainability. Attendees to the event will learn about examples of providers who implemented a new AI-powered model with powerful outcomes
Learning points:
- Learn about the current and upcoming challenges facing the case management/utilization review area and their revenue integrity impact
- Understand the fundamentals of artificial intelligence and its emerging impact on healthcare
- Hear about a health system’s experience and outcomes from implementing a new AI-powered utilization review model
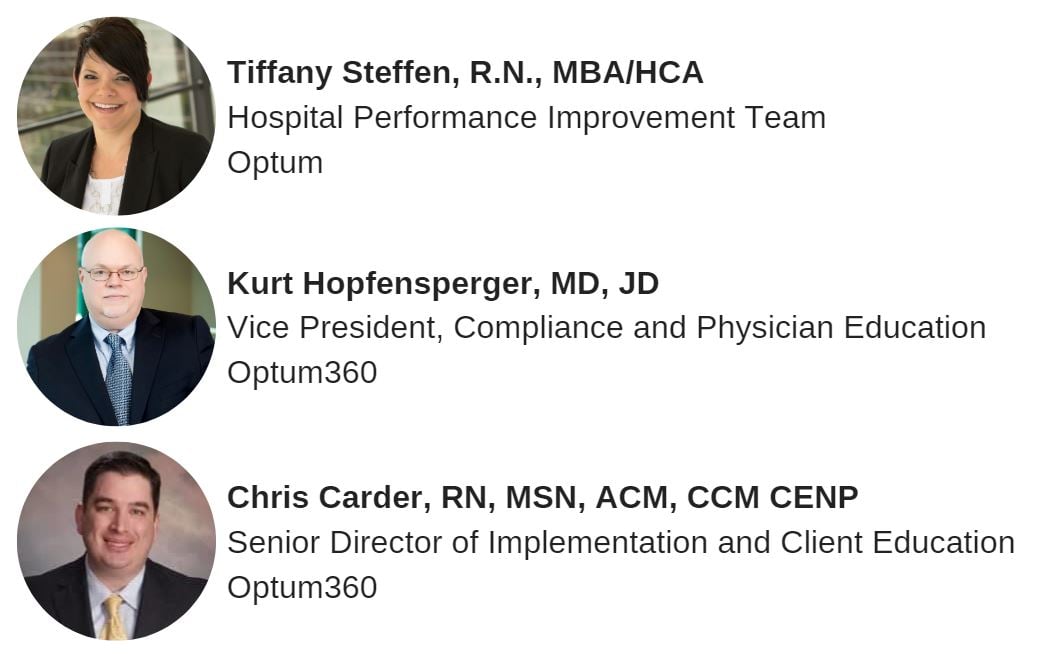
Speakers: